For many couples and individuals, starting a family is one of life’s most cherished goals. But when pregnancy doesn’t happen as expected, questions and concerns naturally arise. Knowing when to seek fertility testing is a crucial first step toward understanding your reproductive health and taking control of your family planning journey.
At Medeor Hospital, Abu Dhabi, we provide compassionate, evidence-based fertility evaluations tailored to your unique needs. In this blog, we explain what fertility testing involves, when it’s time to consider it, and the key signs you shouldn’t ignore.
What is Fertility Testing
Fertility testing refers to a series of medical evaluations designed to identify potential causes of infertility in both men and women. The goal is to assess reproductive health, hormone levels, and physical conditions that may be affecting your ability to conceive.
Testing typically includes:
- Hormone blood tests
- Ovulation tracking
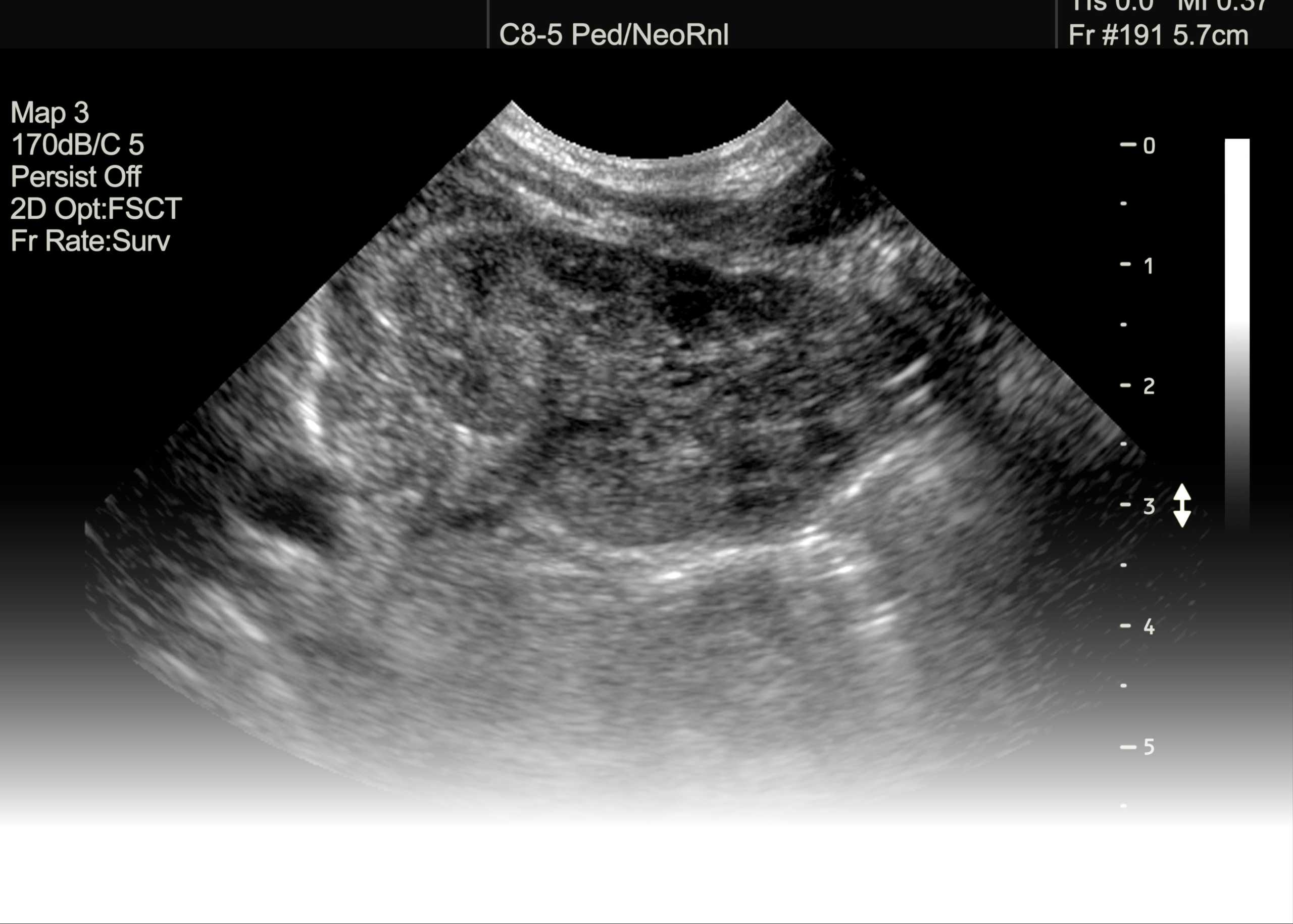
- Ultrasound scans (for ovarian reserve and uterine health)
- Semen analysis (male fertility test)
- Imaging tests like Hysterosalpingography (HSG) to assess fallopian tubes
When Should You Start Fertility Testing
You don’t need to wait years to speak with a specialist. Early diagnosis can lead to quicker solutions and reduce emotional stress. Here’s when experts recommend seeking a fertility evaluation:
1. After 12 Months of Trying (Age <35)
If you’re under 35 and have been having regular, unprotected intercourse for a year without success, it’s time to consider testing.
2. After 6 Months of Trying (Age ≥35)
For women aged 35 and above, it’s advised to begin testing after just six months of trying, as fertility naturally declines with age.
3. Immediately (Age ≥40)
Women aged 40 or older should consult a fertility specialist right away, even before actively trying for several months, due to the more rapid decline in egg quality and quantity.
Key Signs You Should See a Fertility Specialist
Sometimes, even before the typical timeframes, there are early warning signs that signal it’s time for an evaluation.
1. Irregular or Absent Periods
This could indicate issues with ovulation, polycystic ovary syndrome (PCOS), or hormonal imbalances.
2. Painful Periods or Intercourse
Severe menstrual cramps or pain during intercourse may be signs of endometriosis or pelvic inflammatory disease (PID), which can affect fertility.
3. History of Miscarriages
Two or more miscarriages, even in early pregnancy, may point to underlying reproductive or genetic issues.
4. Known Reproductive Conditions
If you’ve been diagnosed with conditions like PCOS, fibroids, or thyroid disorders, early fertility assessment is recommended.
5. Male Factor Concerns
Men with low libido, erectile dysfunction, past testicular trauma, or a history of varicocele should consider semen analysis to evaluate sperm count, motility, and morphology.
6. Previous Pelvic Surgery or Infections
These can affect the uterus, fallopian tubes, or ovaries, impacting your ability to conceive.
7. You’re Planning to Delay Parenthood
If you’re not planning to conceive soon but are concerned about future fertility, egg freezing and fertility preservation options are available and most effective when done earlier.
Why Early Fertility Testing Matters
- Faster Diagnosis: Identifies any underlying conditions sooner.
- Wider Treatment Options: Early detection often leads to less invasive and more cost-effective solutions.
- Emotional Relief: Reduces stress by giving clarity and a clear plan.
- Future Planning: Helps you make informed decisions about egg/sperm preservation if you’re not ready for parenthood yet.
What to Expect During a Fertility Evaluation at Medeor Hospital
At Medeor Hospital, Abu Dhabi, your comfort and clarity are our priorities. Our fertility assessment process includes:
- Comprehensive medical history review
- Personalized lab tests and imaging
- Male and female fertility evaluations
- Emotional and psychological support
- A tailored treatment plan, from natural methods to advanced options like IVF or IUI
Our multidisciplinary team of OB-GYNs, fertility specialists, and endocrinologists work together to give you the best possible chance of success.
Final Thoughts
If you’re wondering when to start fertility testing, the simple answer is: sooner is better. Whether you’re actively trying to conceive or just exploring your reproductive options, early evaluation provides clarity, reassurance, and better outcomes.
Don’t wait in uncertainty. The expert team at Medeor Hospital, Abu Dhabi is here to guide you with care, sensitivity, and advanced diagnostics every step of the way.