Empowering You to Prevent, Detect, and Manage Diabetes Better
Diabetes is one of the most common chronic health conditions today—but it’s also one of the most manageable. With the right knowledge, timely screening, and lifestyle adjustments, people can prevent complications and even delay the onset of diabetes. And thanks to rapid medical innovations, managing diabetes today is far easier and more effective than ever before.
At Medeor Hospital, Abu Dhabi, our specialists in endocrinology, internal medicine, and nutrition are embracing these new technologies to help patients live healthier, fuller lives—without letting diabetes define them.
Understanding Diabetes: The Basics You Should Know
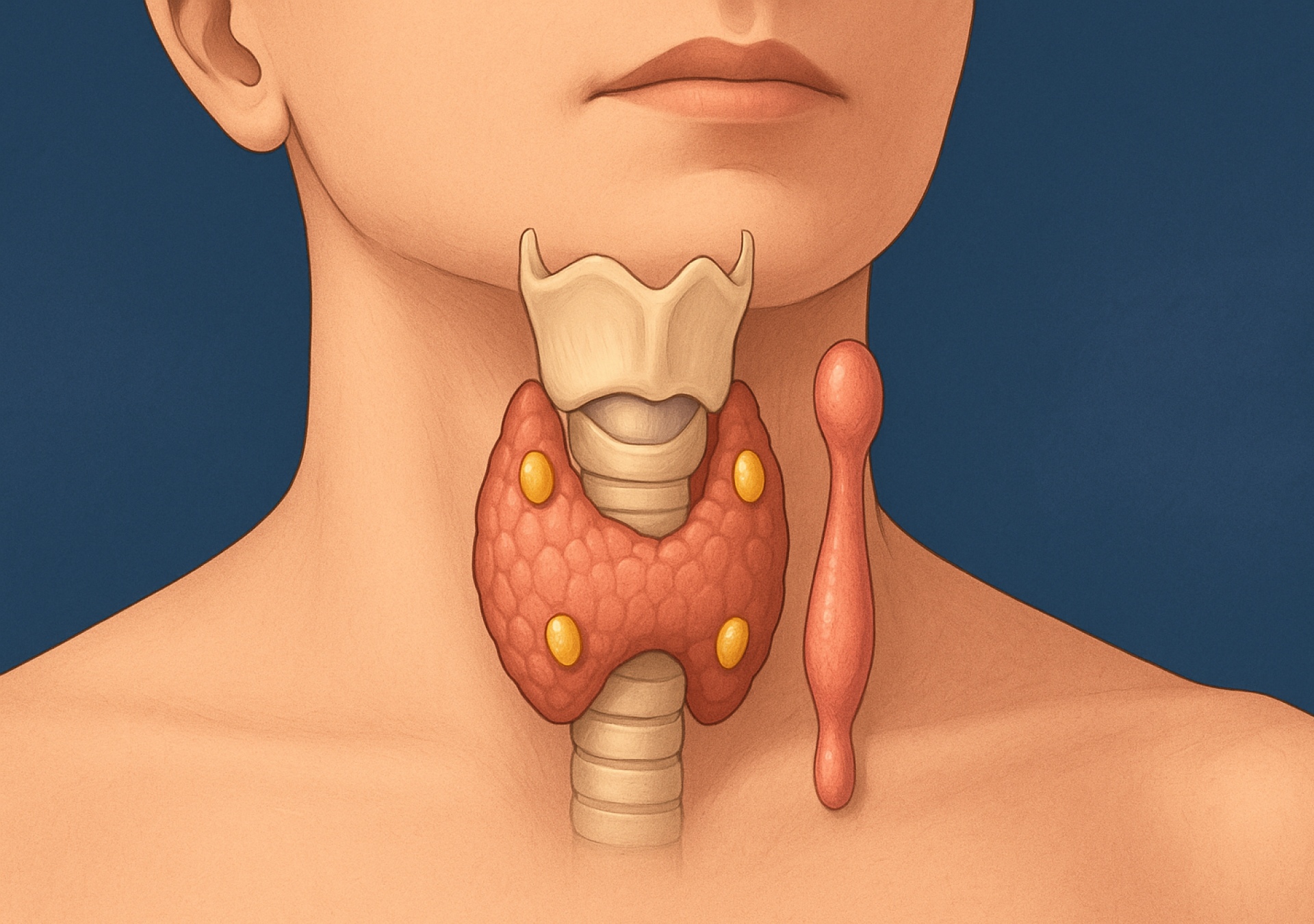
Diabetes occurs when your body either doesn’t produce enough insulin or cannot use it effectively. Insulin is a hormone that regulates blood sugar levels—too little or ineffective use leads to high blood sugar, which can damage organs over time.
The Two Main Types of Diabetes:
- Type 1 Diabetes: The immune system attacks insulin-producing cells. Usually diagnosed in childhood or adolescence.
- Type 2 Diabetes: The body becomes resistant to insulin or produces less of it—often linked to lifestyle, weight, and age.
There’s also prediabetes, a warning stage where blood sugar levels are higher than normal but not yet diabetic. With early lifestyle changes, prediabetes can often be reversed.
Recognizing the Early Warning Signs
The challenge with diabetes is that it often creeps in silently. Many people discover it only after a routine test. However, recognizing early symptoms can make a major difference.
Common Symptoms of Diabetes Include:
- Increased thirst and frequent urination
- Unexplained fatigue or weakness
- Sudden weight loss (especially in Type 1)
- Slow-healing wounds
- Blurred vision
- Frequent infections (such as skin or urinary tract)
If you notice these signs, it’s crucial to get screened early. Regular testing—especially if you have risk factors—helps detect diabetes before complications begin.
Who’s at Risk? Know the Factors
Some risks can’t be changed, but many can be controlled.
Uncontrollable Risk Factors:
- Family history of diabetes
- Age above 40
- Ethnicity (higher prevalence in South Asian and Middle Eastern populations)
Controllable Risk Factors:
- Being overweight or physically inactive
- High blood pressure or cholesterol
- Poor diet (high in sugar and processed food)
- Stress and lack of sleep
Even if diabetes runs in your family, lifestyle changes can dramatically reduce your risk or delay its onset.
Advances in Screening and Diagnosis
Gone are the days when blood tests required long waits and complicated procedures. New technology has made diabetes detection quicker and more accurate.
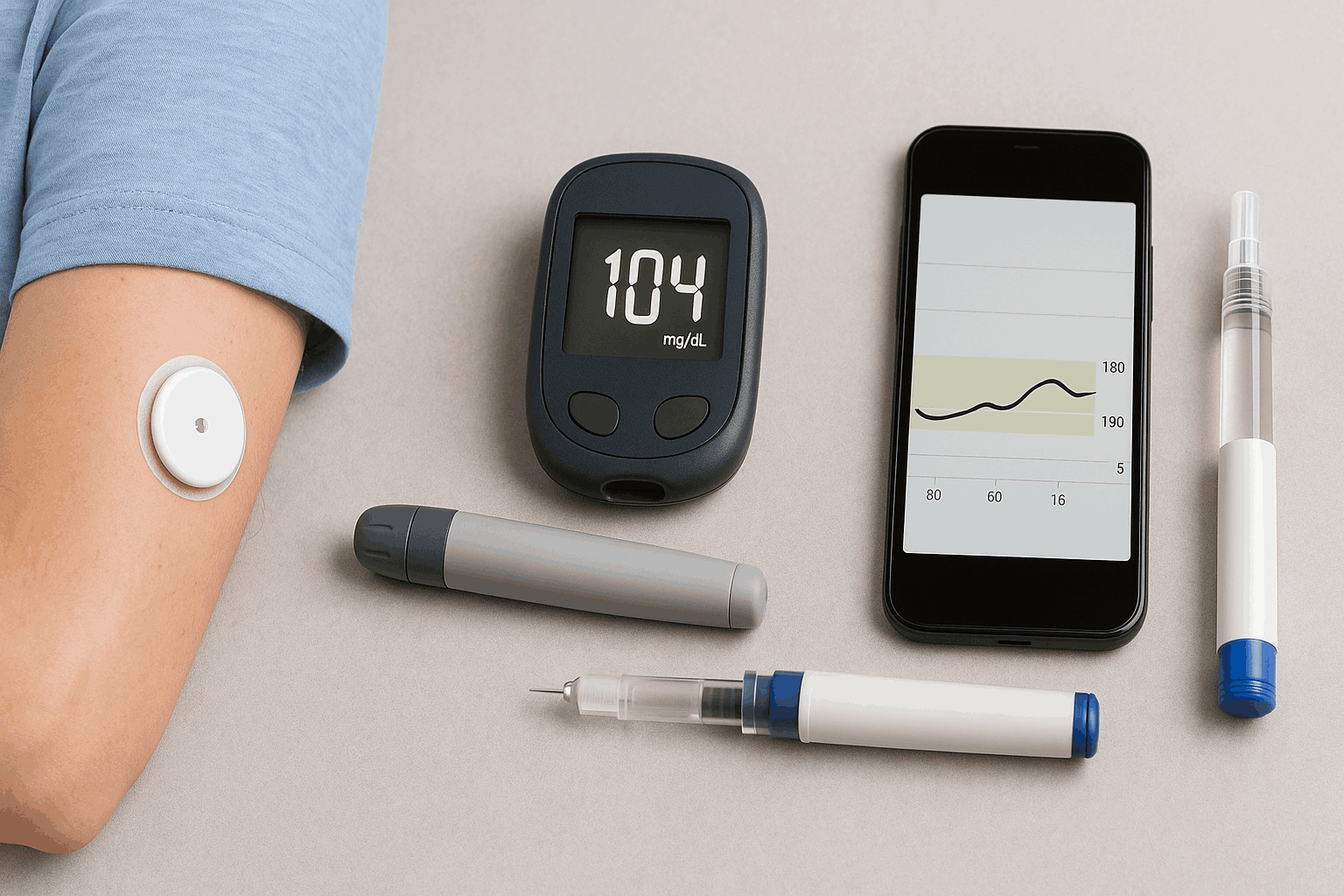
a. Continuous Glucose Monitoring (CGM):
Small sensors placed on the skin continuously track blood sugar levels throughout the day. This helps patients and doctors understand how food, exercise, and stress affect glucose—without frequent finger pricks.
b. Flash Glucose Monitoring:
A simpler alternative, these sensors can be scanned with a smartphone or reader for instant glucose data.
c. Smart Diagnostics:
AI-powered tools now analyze risk factors and test results to predict the likelihood of diabetes earlier than traditional screening.
At Medeor, our diagnostic units are equipped with advanced screening tools that make early detection faster, easier, and more accurate—helping patients take timely action.
Latest Treatment Innovations
Medical science is transforming how diabetes is treated and monitored. Here’s what’s making life easier for patients today:
a. Smart Insulin Pens & Pumps
These devices automatically deliver the right insulin dose and even store data digitally. Some are Bluetooth-enabled and sync with apps, allowing doctors to review patterns remotely.
b. Artificial Pancreas Systems
This revolutionary technology links a glucose monitor with an insulin pump—automatically adjusting insulin levels as needed. It mimics how a healthy pancreas works, reducing the burden of manual tracking.
c. Advanced Medications
Modern drugs like GLP-1 receptor agonists and SGLT2 inhibitors not only help control blood sugar but also support heart and kidney health. They are transforming long-term diabetes care.
d. Telemedicine & Remote Monitoring
Virtual consultations let patients track progress and get personalized advice without frequent hospital visits—especially useful for working professionals or elderly patients.
e. Personalized Nutrition Plans
AI-driven diet tracking and metabolic assessments are now used to design individualized meal plans. At Medeor, our dietitians help create plans that fit your culture, preferences, and daily routine.
Prevention Through Lifestyle: Your Best Defense
Technology helps, but prevention still begins with simple lifestyle habits. Even small, consistent actions can make a huge difference.
Eat Smart
- Include fiber-rich foods like whole grains, legumes, and vegetables.
- Reduce processed sugar and trans fats.
- Choose smaller, more frequent meals to maintain steady energy.
- Stay hydrated—water helps regulate metabolism.
Stay Active
At least 150 minutes of moderate activity a week (like brisk walking, cycling, or swimming) can cut diabetes risk by up to 50%. Even short breaks during long office hours help.
Manage Stress
Chronic stress increases blood sugar. Meditation, deep breathing, and mindful hobbies can lower stress hormones and improve focus.
Get Enough Sleep
Poor sleep affects metabolism and appetite control. Aim for 7–8 hours of quality sleep nightly.
Stop Smoking
Smoking worsens insulin resistance and raises heart disease risk in diabetics. Quitting significantly improves overall health outcomes.
Early Detection: Why Regular Screening Matters
Even if you feel fine, regular check-ups are essential—especially if you fall into a higher-risk category. Diabetes often causes internal changes long before symptoms appear.
Recommended Screening Frequency:
- Every 6–12 months for people with risk factors (obesity, family history, sedentary lifestyle)
- Every 3–6 months for prediabetics or those under treatment
- Annual full-body health checks for adults above 30
At Medeor Hospital, comprehensive Diabetes Health Packages combine blood glucose testing, HbA1c, lipid profile, and kidney function tests—giving patients a clear picture of their metabolic health.
Lifestyle Medicine: The Future of Diabetes Care
Beyond medication, the medical community now focuses on Lifestyle Medicine—an integrated approach combining nutrition, exercise, sleep, and stress management with medical support.
Medeor’s endocrinologists, dietitians, and physiotherapists collaborate to create personalized lifestyle roadmaps, empowering patients to regain control naturally. This approach not only manages diabetes but also prevents complications like neuropathy, eye disease, and heart issues.
The Role of Corporate Wellness
For many working adults, long hours, irregular meals, and stress contribute to rising diabetes cases. Recognizing this, Medeor partners with organizations in Abu Dhabi to promote corporate wellness programs that include:
- Annual diabetes screenings
- On-site nutrition consultations
- Fitness and stress management workshops
- Tailored health packages for employees and families
These initiatives encourage prevention and early detection, creating healthier workforces and reducing absenteeism.
Real Stories of Progress
At Medeor Hospital, we’ve witnessed hundreds of success stories—patients who reversed prediabetes or regained control through lifestyle and technology. One such patient, a 45-year-old corporate employee, managed to bring his HbA1c from 8.4% to 5.9% within six months through a personalized diet plan, CGM tracking, and guided physical therapy.
These stories remind us that every step counts, and with the right support, change is achievable.
How Medeor Hospital Leads the Way
Medeor’s Comprehensive Diabetes Care Program integrates:
- Endocrinology Consultation for medical management
- Diet & Nutrition Counseling tailored to lifestyle and culture
- Diabetic Foot & Eye Care Clinics for early complication detection
- Fitness & Physiotherapy Support for better mobility and strength
- Technology-Assisted Monitoring to track and optimize outcomes
We believe in treating diabetes not just as a condition—but as a journey toward better living.
Take Action Today
Whether you’re living with diabetes, at risk, or simply want to take preventive steps, the key is awareness and consistency. The earlier you act, the easier it is to manage.
Start with these three steps:
- Get screened. Know your numbers—especially blood glucose and HbA1c.
- Move daily. Even small lifestyle changes have big impacts.
- Seek expert guidance. Our doctors and dietitians can help you find a routine that fits your life.
Conclusion: Living Beyond Diabetes
Diabetes doesn’t have to limit your life. With today’s technology, knowledge, and support systems, you can prevent, control, and thrive beyond the diagnosis.
At Medeor Hospital, Abu Dhabi, we are committed to guiding you every step of the way—from awareness to advanced care—because your health journey deserves expert attention and compassionate care.
Prevention starts with you.
Let’s make every step count—toward a healthier, diabetes-free future.