Introduction:
An inborn term neonate weighing 2600 g developed meconium aspiration syndrome (MAS) at birth. The baby experienced respiratory failure requiring high-frequency oscillatory ventilation support. Pulmonary hypertension, along with hypotension and left ventricular dysfunction noted on point-of-care echocardiography (POCE), necessitated a trial of epinephrine and inhaled nitric oxide (iNO). The case was further complicated by bilateral pneumothorax. Despite an extremely complex presentation with severe hypoxemic failure refractory to iNO, a novel treatment plan led to intact survival.
Case Presentation:
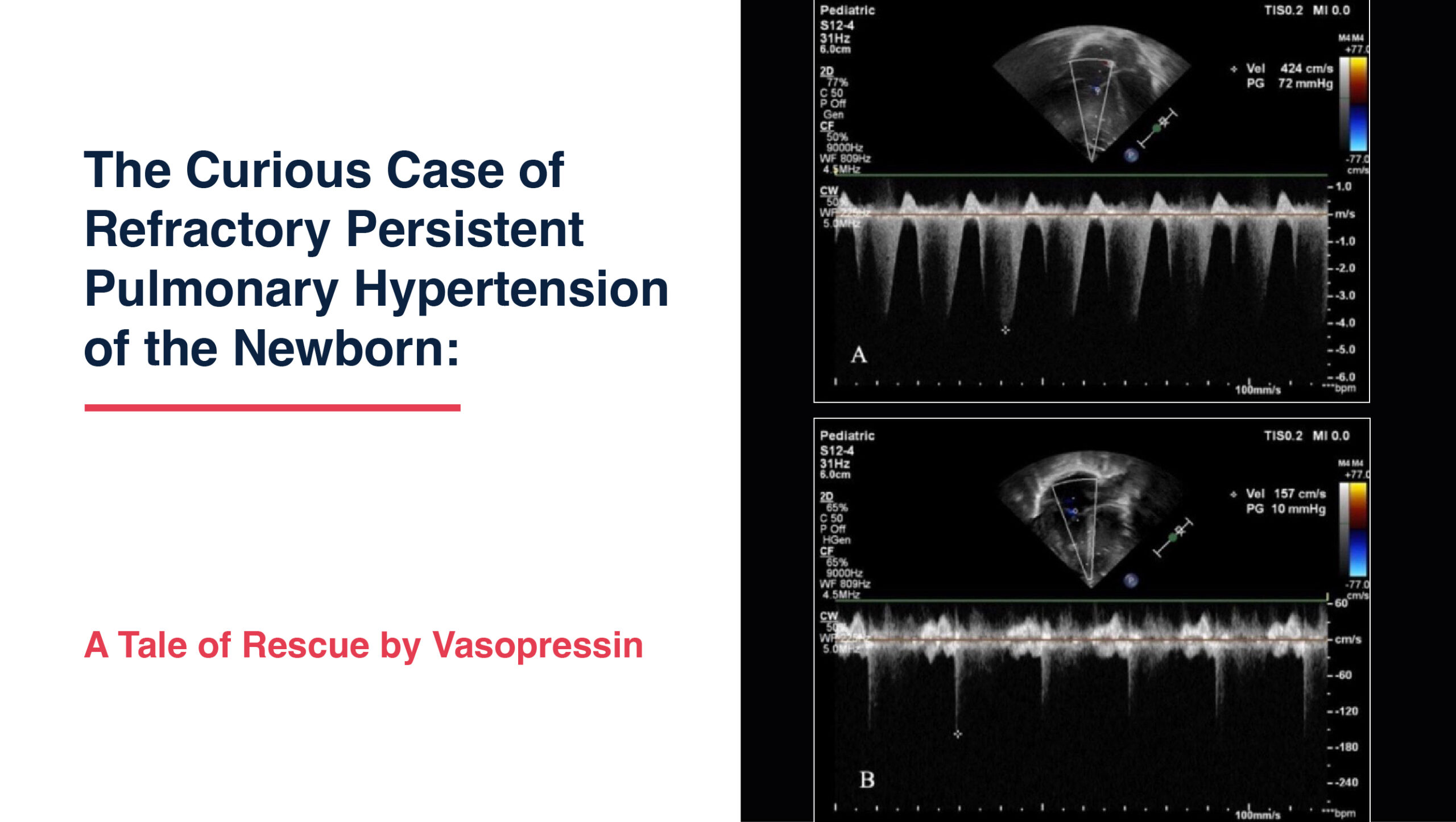
A 37-week, 2600-gram male neonate was delivered by emergency lower segment cesarean section for fetal distress and meconium-stained liquor. The antenatal period was uneventful. The baby developed worsening respiratory distress at 15 hours of life, requiring high-frequency oscillatory (HFO) ventilation with a mean airway pressure as high as 20 cm and an oxygenation index (OI) of 22. Point-of-care functional echocardiography revealed severe PPHN (pulmonary artery pressure 70 mmHg) with left ventricular (LV) dysfunction (LV fractional shortening 18%). Epinephrine was initiated to augment LV contractility, followed by iNO therapy for hypoxemic respiratory failure (HRF) secondary to severe PPHN. However, the baby turned out to be an iNO non-responder.
The Crucial Salvage:
This complex scenario of HRF with hypotension and iNO-refractory PPHN was managed by adding vasopressin infusion, which has a unique combination of vasopressor activity on systemic circulation and vasodilatory action on pulmonary circulation. The addition of vasopressin to iNO therapy helped improve hypotension and reduce pulmonary pressures. The baby also developed bilateral pneumothorax, which was managed with bilateral intercostal drainage. As blood pressure improved with epinephrine, milrinone was added to further improve PPHN due to its ino-dilatory properties.
Outcome:
Following an intricate protocol of epinephrine, iNO, vasopressin, and milrinone in a novel and crucial sequence, along with continuous bedside point-of-care functional echocardiography for monitoring LV function and PPHN, the baby was successfully salvaged and discharged on day 30 of life.
Follow-up:
At 3 months of age, the baby had appropriate weight gain and a completely normal neurological examination without any respiratory issues.
Severe PPHN: Management Strategies in iNO Non-Responders
Inhaled NO is the treatment of choice for pulmonary artery hypertension (PAH) in neonates. However, poor lung development secondary to extraneous contents in the thorax or prolonged suppression of endogenous NO synthase have been postulated as reasons for poor response to iNO. Sildenafil (a phosphodiesterase V inhibitor) and milrinone (a phosphodiesterase III inhibitor) have been used to treat PPHN non-responsive to iNO with variable success rates.
Vasopressin acts on systemic arterial V1 receptors and causes vasoconstriction. By activating pulmonary vascular endothelial nitric oxide synthase through the oxytocin endothelial receptor, it has also been reported to have pulmonary vasodilatory effects. This action helps create a high systemic and low pulmonary vascular resistance (PVR) state, thereby tipping the balance towards a higher systemic vascular resistance (SVR)ratio.
Conclusion:
This case highlights the importance of combining clinical and physiological principles of drug actions and synergisms to treat complicated cases of refractory PPHN with systemic hypotension and hypoxemic respiratory failure. Point-of-care neonatologist-performed echocardiography-based management is crucial for monitoring dynamic changes in neonatal pulmonary and cardiac functions, facilitating physiology-based, timely treatment in critically ill neonates.
Learning Points:
- This case demonstrates the potential of vasopressin in the treatment of severe pulmonary artery hypertension (PAH) that is refractory to inhaled nitric oxide.
- Vasopressin has a favorable effect on both systemic and pulmonary vasculature, unlike other non-selective pulmonary vasodilators (e.g., sildenafil) currently in use.
- Point-of-care neonatologist-performed echocardiography-based management aids in timely and physiology-based management of fragile, sick newborns.